- 3.39 MB
- 2022-04-29 14:40:31 发布
- 1、本文档共5页,可阅读全部内容。
- 2、本文档内容版权归属内容提供方,所产生的收益全部归内容提供方所有。如果您对本文有版权争议,可选择认领,认领后既往收益都归您。
- 3、本文档由用户上传,本站不保证质量和数量令人满意,可能有诸多瑕疵,付费之前,请仔细先通过免费阅读内容等途径辨别内容交易风险。如存在严重挂羊头卖狗肉之情形,可联系本站下载客服投诉处理。
- 文档侵权举报电话:19940600175。
'心脏辅助器械发展-中英文课件
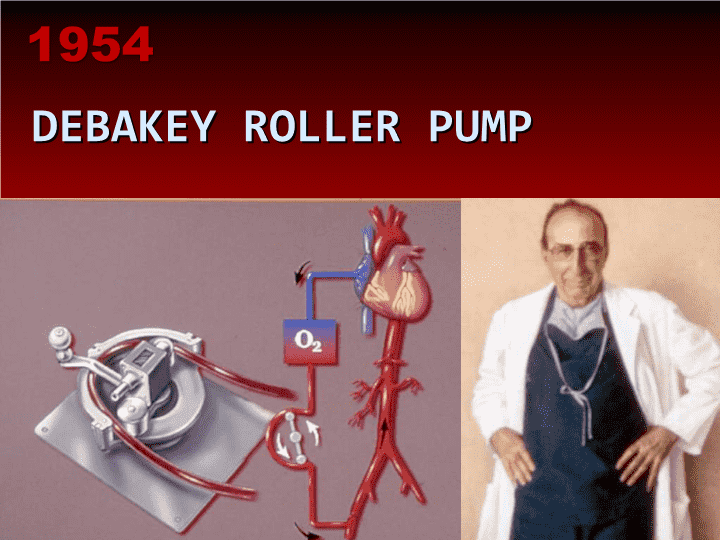
DEBAKEYROLLERPUMP1954
心脏支持辅助装置的发展历史心脏移植前类脉动式装置完全人工或永久性支持设计DeBakeyVAD–1966LiottaTAH–1969AkutsuTAH–1981Jarvik7TAH-1982
AKUTSUTAH的临床植入1981DentonCooley
1982首例永久性TAH植入
里程碑式的转变:FDA通过了(LVAD)作为最终移植前的过渡治疗1984
心脏大小差异带来的技术限制
TCI-THORATECLVADVictorPoirier1984,1986
NOVACOR-WORLDHEARTPeerPortner1984
持续流动装置的出现SarnsBiomedicus
LinearisedRateofRightVentricularFailure0.000.100.200.300.400.500.600-77-1414-30>30DaysafterLVASImplantEvents/Recipient.month
REMATCH试验RandomizedEvaluationofMechanicalAssistancefortheTreatmentofCongestiveHeartFailure充血性心力衰竭机械辅助治疗的随机化评估研究
植入到装置失效时间总体平均时间332天(15-632)流入瓣衰竭408天(240-632)动力装置失效285天(15-439)NumberofDays
通过轴流改进装置的小型化/微型化1998GeorgeNoon
HeartMateII
>2800PatientsImplanted53先期研究488移植前过渡治疗商业性植入Europe:PostCEMarkUS:PostFDAApproval648最终治疗HeartMateII全球临床研究1136主要研究AsofMarch2009n=281(18mofollow-up)Durations413>1year241>1.5year188>2yr42>3yr3>4yr1>5yrDT主要人群随访2年May2009Cohorts:RandomizedvsXVEXVEExchangeSmallptsFDAApprovalApr2008
HeartMateII临床研究有效支持时间(n=281)中位数:155天(最长:5年)平均持续时间:237天181患者年累积支持87%患者出院78%带着支持装置10%在心脏移植后(priortoindexdischarge)77%的使用时间(140例年)为院外使用时间
HeartMateII实际存活曲线Primary(n=133)andCAP(n=146)Cohorts12mo:71±5%6mo:77±4%RemainingatriskPrimary:1334832CAP:1468410PRIMARYCAPAsofSep14,20076mo:87±3%12mo:75±6%PaganietalAHA2007
HeartMateII临床试验移植后存活率移植后30天存活率150/157(96%)移植后一年存活率117/128(91%)
HeartMateII临床研究致死因素(56/281)
HeartMateII临床研究不良事件
HeartMateII临床研究不良事件UseofRVADorextendedinotropeuse>14days,orstartingafter14days
不良事件发生率比较HMII(n=281)vsHMVEBTT(n=280)11Frazier,Rose,OzetalJTCVS2001
HeartMateII无主要装置失效或置换事件率(BTT,n=281)6mo:96±1%12mo:93±2%18mo:92±3%Remainingatrisk2811317252Paganietal(submitted2008)
VentrAssist
VentrAssist
HeartWare
DuraHeart
Matthews-Michigan35%LVAD患者出现右室衰竭共197例患者1996–200668例RV衰竭患者中,58例为植入第一代VAD患者,3例为非脉动式LVAD患者。RV衰竭使LVAD患者的死亡几率增加了6倍
Dang-Columbia39%例出现RV衰竭108patients1996–2004CVP的升高是唯一的独立预测因素
Potapov-Berlin17%RV衰竭54patients1998-2006
Potapov–BerlinRV衰竭的危险因素三尖瓣关闭不全右室的解剖形状RV的后负荷脉动式和持续血流装置间无差异
Fitzpatrick-UPenn37%RV衰竭266patients1995-2007
RVFRSRisk(RV衰竭危险评分)需血管加压素-4分AST>80-2分胆红素>2.0-2.5分肌酐>2.3-3分
AbioCorImplantableComponentsThoracicUnitImplantedControllerImplantedTETCoilImplantedBattery
14例患者入选4个中心12例获得成功心脏支持2例出院支持作用时间:53-512days(17个月)累积支持:5.2例年2例围术期死亡出血—79岁,二次手术,泵工作5小时余肺动脉血栓形成—弥漫的凝血病理改变,应用血液制品
CardioWestTotalArtificialHeart
首例完全人工心脏移植--Dr.BarneyClark
前景如何??完全人工心脏左室辅助装置左室辅助并短期右室辅助装置(Hybrids)双室辅助装置
结论完全人工心脏:从整体生理控制角度考虑,具有一定优势心室辅助装置更容易接受两个泵会2倍增加机械失效几率无论结果怎样,期望辅助装置能更小,能效更高,可靠,植入易行,性价比更高,而且最好能完全植入(患者满意).
英文原版
TheU.S.ExperiencewithTotalArtificialHeartsvs.LeftVentricularAssistDevicesLyleD.Joyce,M.D.,PhD.DivisionofCardiovascularSurgeryTheMayoClinic,Rochester,MN,USA
DEBAKEYROLLERPUMP1954
“Experimentally,itispossibletoreplacetheheartwithanartificialheart,andanimalshavebeenknowntosurviveaslongas36hours.Thisidea,Iamsure,couldreachfullfruitionifwehadmorefundstosupportmorework,particularlyinthebioengineeringarea.”M.DeBakey1963
NATIONALHEARTANDLUNGINSTITUTEESTABLISHEDTHEU.S.ARTIFICIALHEARTPROGRAM1964
WILLEMJ.KOLFF
FIRSTSUCCESSFULLVADBRIDGETORECOVERY1966
HistoryofCardiacSupportDevicesPre-datesCardiacTransplantationPulsatileDevicesDesignedforWeaningorPermanentSupportDeBakeyVAD–1966LiottaTAH–1969AkutsuTAH–1981Jarvik7TAH-1982
CLINICALIMPLANTATION
OFAKUTSUTAH1981DentonCooley
1982FIRSTPERMANENTTAHIMPLANT
ParadigmShift:FDAApprovalForBridgetoTransplantationPriortoUseasDestinationTherapy1984
TECHNICALLIMITATIONSDUETOSIZE
TCI-THORATECLVADVictorPoirier1984,1986
NOVACOR-WORLDHEARTPeerPortner1984
EMERGENCEOF
CONTINUOUSFLOWDEVICESSarnsBiomedicus
LinearisedRateofRightVentricularFailure0.000.100.200.300.400.500.600-77-1414-30>30DaysafterLVASImplantEvents/Recipient.month
REMATCHTrialRandomizedEvaluationofMechanicalAssistancefortheTreatmentofCongestiveHeartFailure
ImplanttoFailureTimeOverallMeanTime332days(15-632)Inflowvalvefailure408days(240-632)MotorMalfunction285days(15-439)NumberofDays
MINIATURIZATIONTHROUGH
AXIALFLOW1998GeorgeNoon
HeartMateII
>2800PatientsImplanted53PilotStudy488BridgetoTransplantCommercialImplantsEurope:PostCEMarkandUS:PostFDAApproval648DestinationTherapyHeartMateIIWorldwideClinicalExperience1136PivotalStudyAsofMarch2009n=281(18mofollow-up)Durations413>1year241>1.5year188>2yr42>3yr3>4yr1>5yrDTprimarycohortwith2yearfollow-upMay2009Cohorts:RandomizedvsXVEXVEExchangeSmallptsFDAApprovalApr2008
HeartMateIIClinicalStudySupportDuration(n=281)Medianduration:155days(longest:5.0yr)Averageduration:237days181pt-yearscumulativesupport87%patientsdischarged78%ondevicesupport10%followingtransplant(priortoindexdischarge)77%oftime(140pt-years)spentoutofhospital
HeartMateIIActuarialSurvival
Primary(n=133)andCAP(n=146)Cohorts12mo:71±5%6mo:77±4%RemainingatriskPrimary:1334832CAP:1468410PRIMARYCAPAsofSep14,20076mo:87±3%12mo:75±6%PaganietalAHA2007
HeartMateIIClinicalTrialPost-transplantSurvival30DaysPost-Transplant150/157(96%)Oneyearpost-transplant117/128(91%)
HeartMateIIClinicalStudyCausesofDeath(56/281)
HeartMateIIClinicalStudyAdverseEvents
HeartMateIIClinicalStudyAdverseEventsUseofRVADorextendedinotropeuse>14days,orstartingafter14days
AdverseEventRateComparisonsHMII(n=281)vsHMVEBTT(n=280)11Frazier,Rose,OzetalJTCVS2001
HeartMateIIFreedomfromMajorDeviceFailureorReplacement(BTT,n=281)6mo:96±1%12mo:93±2%18mo:92±3%Remainingatrisk2811317252Paganietal(submitted2008)
VentrAssist
VentrAssist
HeartWare
DuraHeart
Matthews-Michigan35%RVfailureafterLVAD197Patients1996–2006Of68casesofRVfailure,58occurredinfirstgenerationVAD,3innon-pulsatileLVADPresenceofRVfailureadds6foldincreaseinoddsofpost-opLVADdeath
Dang-Columbia39%RVfailureafterLVAD108patients1996–2004ElevatedCVPwasonlyindependentpredictor
Potapov-Berlin17%RVFailure54patients1998-2006
Potapov–Berlin
RVFailureRiskFactorsTricuspidincompetenceGeometryofRVRVafter-loadNodifferencebetweenpulsatileandcontinuousflowdevices
Fitzpatrick-UPenn37%RVFailure266patients1995-2007
RVFRSRisk
(RVfailureriskscore)Vasopressorrequirement-4pointsAST>80-2pointsBilirubin>2.0-2.5pointsCreat>2.3-3points
AbioCorImplantableComponentsThoracicUnitImplantedControllerImplantedTETCoilImplantedBattery
FourteenPatientsEnrolled
atFourCenters12successfullysupported2dischargedSupportedduration:53-512days(17months)Cumulativesupport:5.2patientyears2perioperativedeathsBleeding—79yr.,reop,5+hr.pumprunPulmonaryarterythrombosis—profoundcoagulopahy,givenfactorconcentrates
CardioWestTotalArtificialHeart
FirstPermanentTotalArtificialHeartImplant--
Dr.BarneyClark
WhatWillTheFutureBe??TotalArtificialHeartsLeftVentricularAssistsLeftVentricularAssistwithshorttermRightVentricularAssist(Hybrids)BiventricularAssists
CONCLUSIONTotalArtificialHeartshavetheadvantagewhenconsideringthevalueoffullphysiologicalcontrolVentricularAssistDeviceshavemoreemotionalappeal.Twopumpscoulddoublethechanceofmechanicalfailure.Whatevertheoutcome,thedevice(s)willhavetobesmall,energyefficient,reliable,easytoimplant,cost-effective,andhopefullytotallyimplantable(patientsatisfaction).
结束语谢谢大家聆听!!!126'
您可能关注的文档
- 最新心脏瓣膜病课件PPT课件
- 最新心脏电复律第八版ppt课件PPT课件
- 最新心脏疾病的超声诊断01PPT课件PPT课件
- 最新心脏疾病的超声诊断02PPT课件PPT课件
- 最新心脏疾病的超声诊断03PPT课件PPT课件
- 最新心脏病人的运动处方ppt课件PPT课件
- 最新心脏的结构课件PPT课件
- 最新心脏肿瘤及心内异常回声课件PPT课件
- 最新心脏课件PPT课件
- 最新心脏除颤复律与起搏ppt课件PPT课件
- 最新心脑血管疾病PPT课件PPT课件
- 最新心脑血管疾病与饮食保健PPT课件PPT课件
- 最新心脑血管疾病知识(商用)PPT课件PPT课件
- 最新心血管xr专升本大课1正常表现ppt课件PPT课件
- 最新心血管危险因素与慢性疾病健康讲座PPT课件PPT课件
- 最新心血管疾病ppt课件PPT课件
- 最新心血管疾病的溶栓、抗栓治疗-教学课件PPT课件
- 最新心血管疾病筛检 PPT课件PPT课件