- 661.00 KB
- 2022-04-29 14:25:14 发布
- 1、本文档共5页,可阅读全部内容。
- 2、本文档内容版权归属内容提供方,所产生的收益全部归内容提供方所有。如果您对本文有版权争议,可选择认领,认领后既往收益都归您。
- 3、本文档由用户上传,本站不保证质量和数量令人满意,可能有诸多瑕疵,付费之前,请仔细先通过免费阅读内容等途径辨别内容交易风险。如存在严重挂羊头卖狗肉之情形,可联系本站下载客服投诉处理。
- 文档侵权举报电话:19940600175。
'培养基的配制
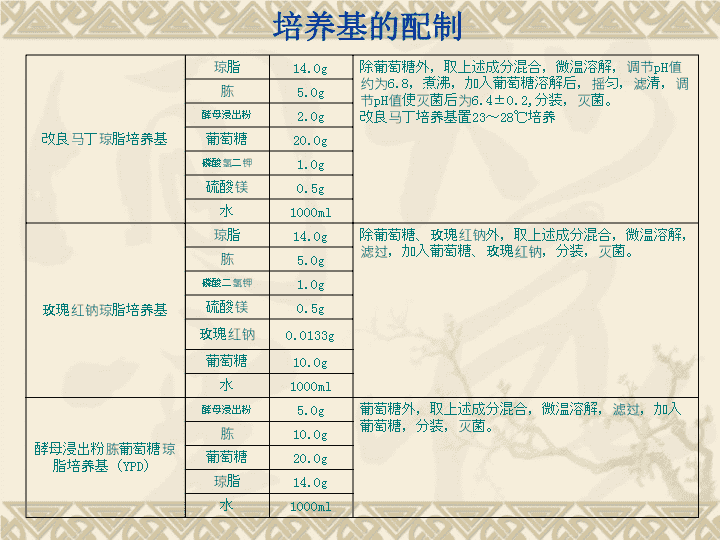
培养基的配制改良马丁琼脂培养基琼脂14.0g除葡萄糖外,取上述成分混合,微温溶解,调节pH值约为6.8,煮沸,加入葡萄糖溶解后,摇匀,滤清,调节pH值使灭菌后为6.4±0.2,分装,灭菌。改良马丁培养基置23~28℃培养胨5.0g酵母浸出粉2.0g葡萄糖20.0g磷酸氢二钾1.0g硫酸镁0.5g水1000ml玫瑰红钠琼脂培养基琼脂14.0g除葡萄糖、玫瑰红钠外,取上述成分混合,微温溶解,滤过,加入葡萄糖、玫瑰红钠,分装,灭菌。胨5.0g磷酸二氢钾1.0g硫酸镁0.5g玫瑰红钠0.0133g葡萄糖10.0g水1000ml酵母浸出粉胨葡萄糖琼脂培养基(YPD)酵母浸出粉5.0g葡萄糖外,取上述成分混合,微温溶解,滤过,加入葡萄糖,分装,灭菌。胨10.0g葡萄糖20.0g琼脂14.0g水1000ml
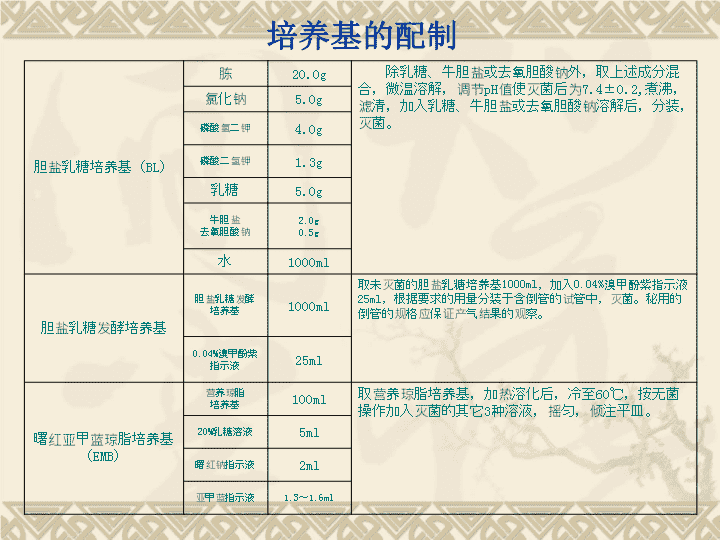
培养基的配制胆盐乳糖培养基(BL)胨20.0g除乳糖、牛胆盐或去氧胆酸钠外,取上述成分混合,微温溶解,调节pH值使灭菌后为7.4±0.2,煮沸,滤清,加入乳糖、牛胆盐或去氧胆酸钠溶解后,分装,灭菌。氯化钠5.0g磷酸氢二钾4.0g磷酸二氢钾1.3g乳糖5.0g牛胆盐去氧胆酸钠2.0g0.5g水1000ml胆盐乳糖发酵培养基胆盐乳糖发酵培养基1000ml取未灭菌的胆盐乳糖培养基1000ml,加入0.04%溴甲酚紫指示液25ml,根据要求的用量分装于含倒管的试管中,灭菌。秘用的倒管的规格应保证产气结果的观察。0.04%溴甲酚紫指示液25ml曙红亚甲蓝琼脂培养基(EMB)营养琼脂培养基100ml取营养琼脂培养基,加热溶化后,冷至60℃,按无菌操作加入灭菌的其它3种溶液,摇匀,倾注平皿。20%乳糖溶液5ml曙红钠指示液2ml亚甲蓝指示液1.3~1.6ml
培养基的配制胆盐硫乳琼脂培养基(DHL)胨20.0g除糖、指示液、琼脂外,取上述成分混合,微温溶解,调节pH值使灭菌后为7.2±0.1,加入琼脂,加热溶化后,再加入其余成分,摇匀,灭菌,冷至约60℃,倾注平皿。牛肉浸出粉3.0g乳糖10.0g蔗糖10.0g去氧胆酸钠1.0g硫代硫酸钠2.3g枸橼酸钠1.0g枸橼酸铁铵1.0g中性红指示液3ml琼脂16.0g水1000ml溴化十六烷基三甲铵琼脂培养基胨10.0g除琼脂外,取上述成分混合,微温溶解,调节pH值,使灭菌后为7.5±0.1,加入琼脂,加热溶化后,分装,灭菌,冷至约60℃,倾注平皿。牛肉浸出粉3.0g氯化钠5.0g溴化十六烷基三甲铵0.3g琼脂14.0g水1000ml
培养基的配制亚碲酸盐肉汤培养基营养肉汤培养基100ml临用前,取灭菌的营养肉汤培养基,每100ml中加入新配制的1%亚碲酸钠(钾)试液0.2ml,混匀,即得。1%亚碲酸钠(钾)0.2ml卵黄氯化钠琼脂培养基胨6.0g除10%氯化钠卵黄液之外,取上述成分混合,微温溶解,调节pH值,使灭菌后为7.5±0.1,灭菌,冷至约60℃,c以无菌操作加入10%氯化钠卵黄液,充分振摇,倾注平皿。10%氯化钠卵黄液的制备:取鲜鸡蛋1个,以无菌操作取卵黄放入10%无菌氯化钠100ml中,摇匀即得。牛肉浸出粉1.8g氯化钠30.0g10%氯化钠卵黄液100ml琼脂14.0g水650ml甘露醇氯化钠琼脂培养基胨10.0g除甘露醇、酚磺酞指示液、琼脂外,取上述成分混合,微温溶解,调节pH值,使灭菌后为7.4±0.2,加入琼脂,加热溶化后,滤过,分装,灭菌,冷至约60℃,倾注平皿。牛肉浸出粉1.0g甘露醇10.0g氯化钠75.0g酚磺酞指示液2.5ml琼脂14.0g水1000ml
培养基的配制乳糖发酵培养基胨20.0g除甘露醇、酚磺酞指示液、琼脂外,取上述成分混合,微温溶解,调节pH值,使灭菌后为7.4±0.2,加入指示液,分装于含倒管的小试管中,每管3ml。灭菌。乳糖10.0g0.04%溴甲酚紫指示液25ml水1000ml绿脓菌素(Pyocyanin)测定用培养基(PDP琼脂培养基)胨20.0g取胨、氯化镁、硫酸钾和水混合后,微温溶解,调节pH值使灭菌后为7.3±0.1,加入甘油及琼脂,加热溶化后,混匀,分装于试管,灭菌,置成斜面。氯化镁(无水)1.4g硫酸钾(无水)10.0g甘油10ml琼脂14.0g水1000ml庖肉培养基取新鲜牛肉,除去脂肪和筋腱,加蒸馏水煮沸约10分钟,切成约5mm3的小块,称重,按1:3(肉:水)加蒸馏水,置4~10℃浸18~20小时后,煮沸1小时,用白布过滤(滤液即为1:3牛肉浸液),肉渣用自来水漂洗2次,然后加入适氢氧化钠溶液,搅拌,使pH在8.4左右,浸泡过夜,次日倒去上层水,用蒸馏水冲洗2~3次,放在纱布上,自动沥干(不要挤压)。将肉渣铺在搪瓷盘上,灭菌,于801~00℃烘干,筛去碎屑,装瓶,保持干燥,备用。庖肉培养基制备将上述碎肉块装入合适的容器中,再加入营养肉汤培养基,碎肉的量约为1.5%,调节pH使灭菌后为7.3±0.1。灭菌。
培养基的配制哥伦比亚培养基酪蛋白胰酶消化物10.0g除琼脂外,取上述成分混合,微温溶解,调节pH值,使灭菌后为7.3±0.2,加入琼脂,加热溶化后,滤过,分装,灭菌,冷至约45~50℃,加入相当于20mg庆大霉素的无菌硫酸庆大霉素,混匀,倾注平皿。心胰酶消化物3.0g玉米淀粉1.0g琼脂15.0g肉胃酶消化物5.0g酵母浸出粉5.0g氯化钠5.0g水1000ml培养基1胨5.0g除琼脂外,取上述成分混合,微温溶解,调节pH值,比最终的pH值高0.2~0.4,加入琼脂,加热溶化后,滤过,调节pH值,使灭菌后为7.8~8.0或6.5~6.6分装,灭菌,牛肉浸出粉3.0g磷酸氢二钾3.0g琼脂15~20g水1000ml
培养基的配制培养基2胨6.0g除琼脂、葡萄糖外,取上述成分混合,微温溶解,调节pH比最终的pH值高0.2~0.4,加入琼脂,加热溶化后,滤过,加葡萄糖溶解后,再调pH值,使灭菌后为7.8~8.0或6.5~6.6分装,灭菌牛肉浸出粉1.5g酵母浸出粉6.0g葡萄糖1g琼脂15~20g水1000ml培养基3胨5.0g除葡萄糖外,取上述成分混合,微温溶解,滤过,加葡萄糖溶解后,调节pH值,使灭菌后为7.0~7.2,灭菌牛肉浸出粉1.5g酵母浸出粉3.0g葡萄糖1g氯化钠3.5g磷酸氢二钾3.68g磷酸二氢钾1.32g水1000ml
培养基的配制培养基4胨5.0g除琼脂、葡萄糖外,取上述成分混合,微温溶解,调节pH值比最终的pH值高0.2~0.4,加入琼脂,加热溶化后,滤过,加葡萄糖溶解后,调节pH值,使灭菌后为6.0~6.8,灭菌氯化钠3.5g葡萄糖1g琼脂15~20g枸橼酸钠8.5gg水1000ml培养基5胨10g除琼脂、麦牙糖外,取上述成分混合,微温溶解,调pH值略高0.2~0.4,加入琼脂,加热溶化后,滤过,加麦牙糖溶解后,调pH值,使灭菌后为7.2~7.4,分装,灭菌琼脂15~20g水1000ml麦牙糖40g培养基6胨8g除琼脂、葡萄糖外,取上述成分混合,微温溶解,调节pH值比最终的pH值高0.2~0.4,加入琼脂,加热溶化后,滤过,加葡萄糖溶解后,调节pH值,使灭菌后为7.2~7.4,灭菌牛肉浸出粉3g氯化钠45g葡萄糖2.5g磷酸氢二钾3.3g磷酸二氢钾1g酵母浸出粉5g琼脂15~20g水1000ml
培养基的配制培养基7胨5.0g除琼脂外,取上述成分混合,微温溶解,调节pH值比最终的pH值高0.2~0.4,加入琼脂,加热溶化后,滤过,调节pH值,使灭菌后为6.5~6.6,灭菌牛肉浸出粉1.5g磷酸氢二钾3.3g磷酸二氢钾1g枸橼酸钠8.5gg琼脂15~20g水1000ml培养基8酵母浸出粉1g取上述成分混合,加热溶化后,滤过,灭菌。琼脂15~20g葡萄糖5g硫酸铵1g磷酸盐缓冲液(pH6.0)1000ml
培养基的配制多黏菌素培养基蛋白胨6.0g除琼脂外,取上述成分混合,微温溶解,调节pH值比最终的pH值高0.2~0.4,加入琼脂,加热溶化后,滤过,调节pH值,使灭菌后为6.5~6.7,灭菌牛肉浸膏1.5g胰消化酪素4.0g葡萄糖1.0g酵母浸膏3.0琼脂15~20g水1000ml
呼吸机治疗的肺保护策略浙江大学医学院附属儿童医院施丽萍
呼吸机相关性肺损伤acuteparenchymallunginjuryandanacuteinflammatoryresponseinthelung.cytokines→alveoliandthesystemiccirculation→multipleorgandysfunctionmortality↑
呼吸机相关性肺损伤
ventilator-inducedlunginjury容量性损伤Volutrauma(largegasvolumes)压力性损伤Barotrauma(highairwaypressure)不张性损伤Atelectotrauma(alveolarcollapseandre-expansion)生物性损伤Biotrauma(increasedinflammation)
肺损伤病理alveolarstructuraldamagepulmonaryedema、inflammation、fibrosissurfactantdysfunctionotherorgandysfunctionexacerbatethedisturbanceoflungdevelopmentSeminNeonatol.2002Oct;7(5):353-60.
ApproachesinthemanagementofacuterespiratoryfailureinchildrenprotectiveventilatoryandpotentialprotectiveventilatorymodeslowertidalvolumeandPEEPpermissivehypercapniahigh-frequencyoscillatoryventilationairwaypressurereleaseventilationpartialliquidventilationimproveoxygenationrecruitmentmaneuverspronepositioningkinetictherapyreduceFiO2andfacilitategasexchangeinhalednitricoxideandsurfactantCurrOpinPediatr.2004Jun;16(3):293-8.
Canmechanicalventilationstrategiesreducechroniclungdisease?continuouspositiveairwaypressurepermissivehypercapniapatient-triggeredventilationvolume-targetedventilationproportionalassistventilationhigh-frequencyventilationSeminNeonatol.2003Dec;8(6):441-8
小潮气量和呼气末正压lowertidalvolumeandPEEP
VentilationwithlowertidalvolumesversustraditionaltidalvolumesinadultsforALIandARDS1202patientslowertidalvolume(≤7ml/kg)lowplateaupressure≤30cmH2Oversustidalvolume10to15ml/kgMortalityatday28long-termmortalitywasuncertainlowandconventionaltidalvolumewithplateaupressure≤31cmH2OwasnotsignificantlydifferentCochraneDatabaseSystRev.2004;(2):CD003844
Higherversuslowerpositiveend-expiratorypressuresinpatientswiththeacuterespiratorydistresssyndrome549patientsacutelunginjuryandARDSlower-PEEPgroup8.3±3.2cmH2Ohigher-PEEPgroup13.2±3.5cmH2O(P<0.001).tidal-volume6ml/kgend-inspiratoryplateau-pressure≤30cmH2OTheratesofdeath24.9%27.5%(p=0.48)Fromday1today28,breathingwasunassisted14.5±10.4days13.8±10.6days(p=0.5)clinicaloutcomesaresimilarwhetherlowerorhigherPEEPlevelsareused.NEnglJMed.2004Jul22;351(4):327-36.
Increasinginspiratorytimeexacerbatesventilator-inducedlunginjuryduringhigh-pressure/high-volumemechanicalventilationSprague-Dawleyratsnegativecontrolgrouplowpressures(PIP=12cmH2O),rate=30,iT=0.5,1.0,1.5secsexperimentalgroupshighpressures(PIP=45cmH2O),rate=10,iT=0.5,1.0,1.5secslungcompliance,PaO2/FiO2ratio,wet/drylungweight,anddrylung/bodyweightasinspiratorytimeincreased,staticlungcompliance(p=.0002)andPao2/Fio2(p=.001)decreased.Wet/drylungweights(p<.0001)anddrylung/bodyweights(p<.0001)increasedLightmicroscopyrevealedevidenceofintra-alveolaredemaandhemorrhageintheiT=1.0andiT=1.5animalsbutnottheLoPandiT=0.5animals.CritCareMed.2002Oct;30(10):2295-9.
新生儿呼吸窘迫综合征
呼吸机治疗的肺保护性策略研究施丽萍孙眉月杜立中中华儿科杂志2003
本项目研究的目的通过肺力学参数的监测(PM)指导呼吸机参数的调节来降低呼吸机相关性肺损伤的发生探讨新生儿RDS最合适的呼吸机参数允许性高碳酸血症对新生儿的影响
非肺力学监测组(NPM):1994~1997年,RDS50例,作为对照组肺力学监测组(PM):1998~2001年,RDS60例,作为观察组肺力学监测仪(BicoreCP100)
两组胎龄、体重、病情严重程度比较胎龄(周)体重(kg)日龄(天)AaDO2(mmHg)a/ANPM32.6±2.11.76±0.35.6±5.1328±1410.16±0.1PM32.7±2.51.89±0.54.8±4.9345±1240.16±0.1t0.1781.6370.7750.6270.597p>0.05>0.05>0.05>0.05>0.05
对照组(NPM):应用人工呼吸机限压定时持续气流型,通气模式为IMV,持续脉搏血氧饱和度监测使其维持在85~95%,每8h监测动脉血气一次,要求血气维持在正常范围内,PaO240-70mmHg,PaCO235-45mmHg
观察组(PM组):1、肺力学监测仪(BicoreCP100)每8~12h监测一次机械通气时肺力学参数2、监测时要求患儿与呼吸机完全同步或无自主呼吸状态(必要时通过药物抑制呼吸)3、肺力学监测仪的传感器置于近端接口4、气管插管气漏率小于20%5、每监测一次持续0.5~1h至数据稳定后记录监测的数据
NPM组和PM组的评估指标1.疾病极期,即生后24~48h时呼吸机要求最高值,包括FiO2、PIP、PEEP、Ti、MAP、VR2.VE、C20/C、TC(限于PM组),3.记录血pH、PaO2、PaCO2、氧合指数(OI)(OI=FiO2×MAP/PaO2)和心率、血压4.呼吸机应用时间,用氧时间,住院天数,病死率,PDA,IVH和呼吸机相关性肺损伤的发生率。
两组呼吸机参数比较FiO2(%)PIP(cmH2O)PEEP(cmH2O)MAP(cmH2O)Ti(sec)VR(次/分)NPM60±1930.5±3.45.6±0.814.9±3.40.75±0.139±9PM62±1826.7±1.75.4±0.611.9±2.00.45±0.142±10t0.1847.5271.3395.81818.101.81p>0.05<0.001>0.05<0.001<0.001>0.05
两组血气监测结果比较PHPaO2(mmHg)PaCO2(mmHg)HR(次/分)BP(mmHg)OINPM7.31±0.157±1740±10144±840±4.619±13PM7.3±0.0459±1648±6.3145±639±3.614±7.7t0.2890.5164.6630.7980.9422.011p>0.05>0.05<0.001>0.05>0.05<0.05
两组呼吸机相关性肺损伤、PDA、IVH、
呼吸机应用时间、用氧时间、住院天数、病死率比较VALI%PDA%IVH%IMV(d)用氧时间(d)住院天数(d)病死率%NPM3236423.9±1.811±719±1414PM13.333.3404.2±1.713±722±118.3t0.8671.4741.22χ²5.570.090.050.9p<0.05>0.05>0.05>0.05>0.05>0.05>0.05
结论肺力学监测能指导正确应用呼吸机,降低呼吸机相关性肺损伤从本研究结果推荐RDS呼吸机应用的参数为:PIP25cmH2O左右,短Ti0.3~0.5秒,应用适当的PEEP5-7cmH2O治疗RDS,不影响氧合。PaCO2的轻度增高(PaCO245-60),IVH的发生未见增加。
允许性高碳酸血症Permissivehypercapnia
Permissivehypercapnia--roleinprotectivelungventilatorystrategiesFirst,weconsidertheevidencethatprotectivelungventilatorystrategiesimprovesurvivalandweexplorecurrentparadigmsregardingthemechanismsunderlyingtheseeffectsSecond,weexaminewhetherhypercapnicacidosismayhaveeffectsthatareadditivetotheeffectsofprotectiveventilationThird,weconsiderwhetherdirectelevationofCO2,intheabsenceofprotectiveventilation,isbeneficialordeleteriousFourth,weaddressthecurrentevidenceregardingthebufferingofhypercapnicacidosis
Lung-protectiveventilationinacuterespiratorydistresssyndrome:protectionbyreducedlungstressorbytherapeutichypercapnia?hypercapnicacidosislung-protectiveventilationrespiratoryacidosisprotectedthelungTheprotectiveeffectofrespiratoryacidosisinhibitionofxanthineoxidasepreventedbybufferingtheacidosis.theprotectionresultedfromtheacidosisratherthanhypercapniaAmJRespirCritCareMed.2000Dec;162(6):2021-2.
PermissivehypercapniainARDSanditseffectontissueoxygenationTheright-shiftofthehaemoglobin-oxygendissociationcurvereduceintrapulmonaryshunt(Qs/Qt)bypotentiatinghypoxicpulmonaryvasoconstrictionaffectthedistributionofsystemicbloodflowbothwithinorgansandbetweenorgansActaAnaesthesiolScandSuppl.1995;107:201-8
HypercapnicacidosisattenuatesendotoxininducedacutelunginjuryattenuatedthedecrementinoxygenationimprovedlungcompliancereducedalveolarneutrophilinfiltrationandhistologicindicesoflunginjuryAmJRespirCritCareMed.2004Jan1;169(1):46-56
Hypercapnicacidosisisprotectiveinaninvivomodelofventilator-inducedlunginjury12rabbitsventilator-inducedlunginjury(VILI)PaCO240mmHgn=6PaCO280-100mmHgn=6respiratorymechanics(plateaupressures)27.0±2.520.9±3.0p=0.016gasexchange(PaO2)165.2±19.477.3±87.9p=0.02wet:dryweight9.7±2.36.6±1.8p=0.04bronchoalveolarlavagefluidproteinconcentration1350±228656±511p=0.03cellcount6.86x1052.84x105p=0.021injuryscore7.0±3.30.7±0.9p<0.0001AmJRespirCritCareMed.2002Aug1;166(3):403-8
EffectsofhighPCO2onventilatedpretermlamblungsPretermsurfactant-treatedlambswithahightidalvolume(Vt)30minacutelunginjury.Vt6-9mL/kg5.5hPCO240-50mmHgaddtotheventilatorcircuitPCO295±5mmHgheartratesbloodpressuresplasmacortisolvaluesoxygenationnodifferent↑whitebloodcells↑hydrogenperoxideproduction↑IL-1beta,IL-8cytokinemRNAexpressionincellsfromthealveolarwashHistopathologylesslunginjuryPediatrRes.2003Mar;53(3):468-72.
PermissivehypercapniaforthepreventionofmorbidityandmortalityinmechanicallyventilatednewborninfantsTwotrialsinvolving269newborninfantsnoevidence↓theincidenceofdeathorCLDat36weeks(RR0.94,95%CI0.78,1.15)noevidence↑IVH3or4(RR0.84,95%CI0.54,1.31)noevidence↑PVL(RR1.02,95%CI0.49,2.12).noevidence↑LongtermneurodevelopmentaloutcomesOnetrialreportedthatpermissivehypercapniareducedtheincidenceofCLDinthe501to750gramsubgroupCochraneDatabaseSystRev.2001;(2):CD002061
Permissivehypercapniainneonates:thecaseofthegood,thebad,andtheuglyPaCO2levelsof45-55mmHginhigh-riskneonatesare"safe"and"welltolerated"PediatrPulmonol.2002Jan;33(1):56-64
高频震荡通气High-frequencyoscillatoryventilation
High-frequencyoscillatoryventilationforacuterespiratorydistresssyndromeinadultpatients148randomized,controlledtrialARDSHFOVPCVPaO2/FiO2<16h(p=0.008)>72hnoThirty-daymortality37%or52%(p=0.102)barotrauma,hemodynamicinstability,ormucuspluggingnodifferentclinicaluseinadultsFiO2>60%andMAP20cmH2OorPEEP>15cmH2OCritCareMed.2003Apr;31(4Suppl):S317-23
ElectivehighfrequencyoscillatoryventilationversusconventionalventilationforacutepulmonarydysfunctioninpreterminfantsupdatedinMay20033275RandomizedcontrolledtrialscomparingHFOVandCVinpretermorlowbirthweightinfantswithpulmonarydysfunctionnoevidenceofeffectonCLDandmortalityat28-30daysPre-specifiedsubgroupanalysesShorttermneurologicalmorbidityGrade3or4IVHandPVL(nousinghighvolumestrategy)CochraneDatabaseSystRev.2003(4):CD000104
OpenlungventilationimprovesgasexchangeandattenuatessecondarylunginjuryinapigletmodelofmeconiumaspirationProspective,randomizedanimalstudy36newbornpiglets(6salinecontrols)PPV(OLC),HFOV(OLC),PPV(CON)ventilatedfor5hrsbronchoalveolarlavagefluidmyeloperoxidaseactivitylunginjuryscoreAlveolarproteininfluxnodifferentsuperioroxygenationandlessventilator-inducedlunginjuryCritCareMed.2004Feb;32(2):443-9
ChangesinmeanairwaypressureduringHFOVinfluencescardiacoutputinneonatesandinfants14patients<1yearweight<10kgHFOVstudygroup(n=9)MAP+5and-3cmH2Ocontrolgroup(n=5)CardiacoutputechocardiographyDopplertechniqueCardiacoutputthestudygroup(P=0.02)thegreatestchangeatthehighestPawat-11%(range:-19to-9)comparedwithbaseline.ActaAnaesthesiolScand.2004Feb;48(2):218-23
Randomizedtrialofhigh-frequencyoscillatoryventilationversusconventionalventilation:effectonsystemicbloodflowinverypreterminfants43infants<29w<1hrwithHFOVorCVAt31024hrsofageEchocardiographySuperiorvenacavaflowRightventricularoutputHypotentionNosignificantadverseeffectsofHFOVonsystemicbloodflowJPediatr.2003Aug;143(2):192-8
气道压力释放通气Airwaypressurereleaseventilation
Airwaypressurereleaseventilationinpediatrics33infantsweight>8kgVitalsigns,airwaypressures,minuteventilation,Spo(2),andE(T)CO(2)wererecordedAPRVprovidedsimilarventilation,oxygenation,meanairwaypressure,hemodynamics,andpatientcomfortasSIMVAPRVsignificantlylowerinspiratorypeakandplateaupressuresPediatrCritCareMed.2001Jul;2(3):243-6
Airwaypressurereleaseventilationasaprimaryventilatorymodeinacuterespiratorydistresssyndrome58patientsrandomizedAPRVorSIMVPIPatAPRV-group(25.9±0.6vs.28.6±0.7cmH2O)(P=0.007).nodifferentPEEPandphysiologicalvariables(PaO2/FiO2,PaCO2,pH,minuteventilation,meanarterialpressure,cardiacoutput)Atday28,thenumberofventilator-freedayswassimilar(13.4±1.7,12.2±1.5),themortality(17%and18%)APRVdidnotdifferfromSIMVwithPSinclinicallyrelevantoutcomeActaAnaesthesiolScand.2004Jul;48(6):722-31
APRVNoevidencetoindicatethatAPRVisbetterthanconventionalventilation
谢谢'
您可能关注的文档
- 最新地磁导航原理与算法研究PPT课件PPT.ppt
- 最新地理必修1第一章地球公转湘教版课件PPT.ppt
- 最新均匀带电圆盘轴线上一点的场强课件PPT.ppt
- 最新垃圾食品(辣条和香肠)的制作过程课件PPT.ppt
- 最新埃及的金字塔ppt课件课件PPT.ppt
- 最新型钢梁的设计课件PPT.ppt
- 最新培优选练(五)-二元一次方程组的同解、错解、参数问题课件PPT.ppt
- 最新城镇燃气输配工程施工及验收规范课件课件PPT.ppt
- 最新培智第五册-08-第八课-细嚼慢咽课件PPT.ppt
- 最新基于MATLAB的信号波形与频谱分析课件PPT.ppt
- 最新基于ANSYS的框架结构风荷载分析..课件PPT.ppt
- 最新基于增强现实ar装配系统研究课件PPT.ppt
- 最新基因的概念及发展课件PPT.ppt
- 最新基因表达-复习课课件PPT.ppt
- 最新基数词与序数词课件PPT.ppt
- 最新基本尺寸孔轴课件PPT.ppt
- 最新基本体的表面交线1分析课件PPT.ppt
- 最新基础会计(东北财大)课件第四章账户与复式记账课件PPT.ppt